AI FOR HEALTHCARE PAYERS
Reduce Administrative Burden in Member and Provider Calls
Observe.AI helps payer contact centers automate repetitive administrative workflows, guide agents in real time, and surface insights that improve accuracy, reduce cost, and speed resolution across high-volume member and provider interactions.
































Here’s how healthcare payers use Observe.AI
24/7 white-glove assistance
Fully automate your high-volume, complex member interactions with empathetic AI agents that understand and solve your members’ health insurance needs in 25+ languages and dialects.
- Coverage and benefits questions
- In-network provider search
- Prescription costs
- Member portal or app support

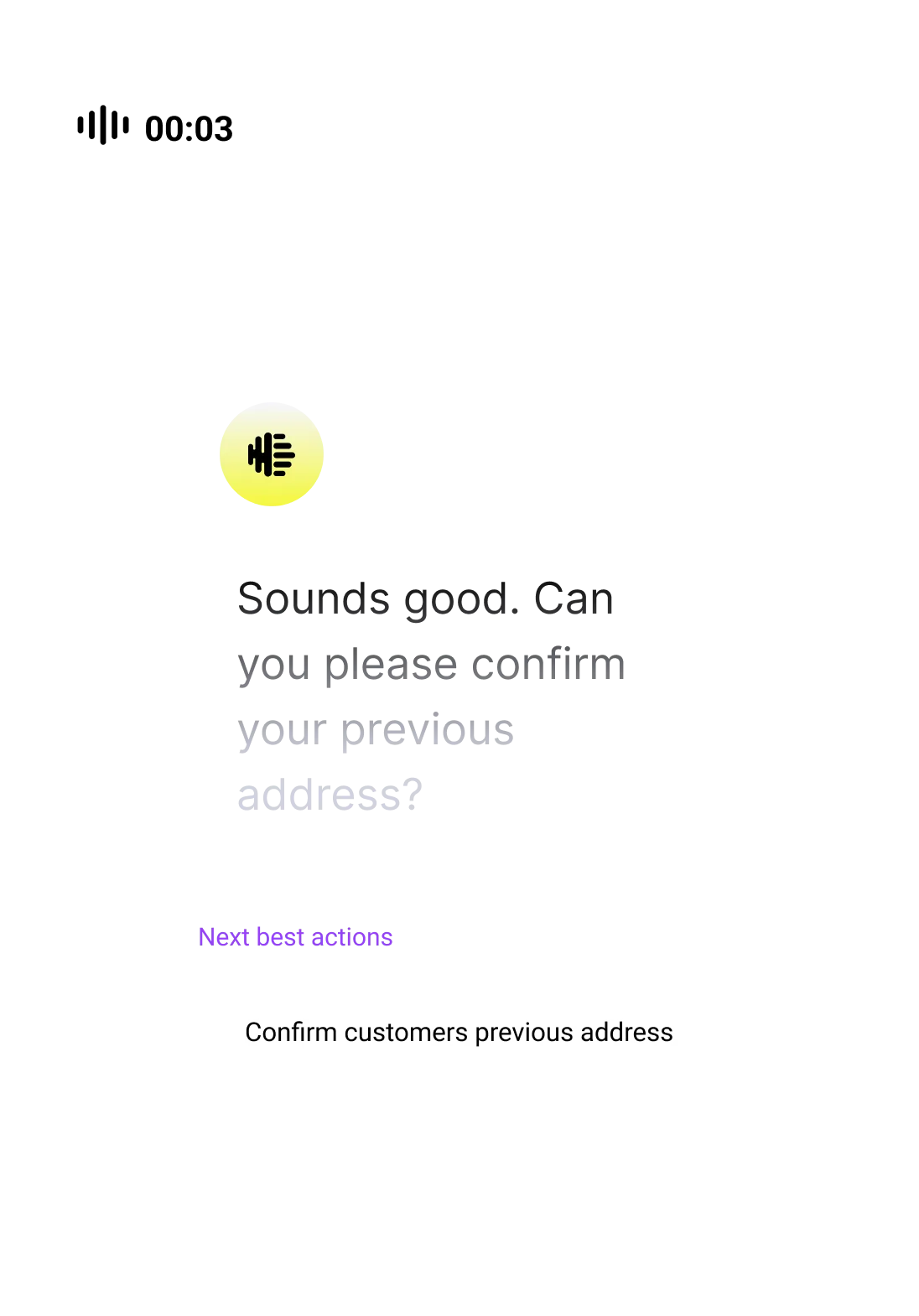
Co-pilot for your team
Help your care service representatives deliver more compassionate and personalized experiences to members in need by offloading compliance, validation, and first-touch engagement steps to AI agents.
- Enrollment in wellness programs
- Medical data entry
- Claims adjudication
- Prior authorization forms
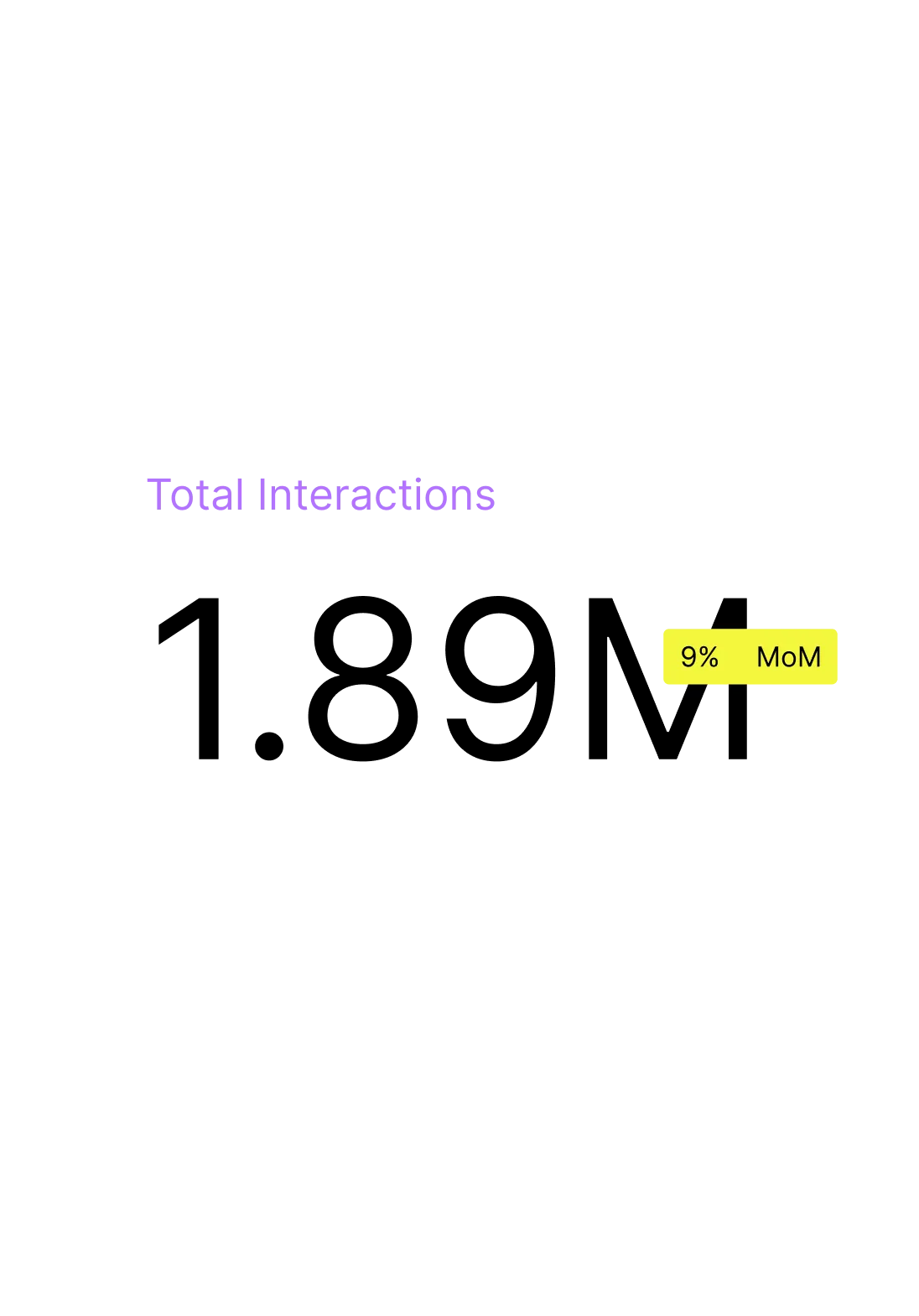
Improved care operations
Analyze 100% of all interactions to continuously improve your AI agent care delivery and adapt data-driven strategies that reduce operational costs and compliance risks while enhancing member outcomes.
- Identify compliance risks
- Product and services gaps
- Care agent performance
- Customer attrition reasons
Seamless integration with your payer systems
Connect your AI Agents to the tools your teams already use
View all integrations




Why healthcare payers prefer Observe.AI
01
01
Trusted Partner
As experts in customer experience with a deep understanding of human-to-human conversations, we work with you to identify more opportunities to seamlessly integrate AI Agents into your organization to address immediate needs with measurable results and drive long-term success.
02
02
Agentic Architecture
Easily create sophisticated AI agents that reflect your brand personality using natural language prompts. Your agents will accurately follow your processes and can take action by connecting with 250+ business systems.
03
03
AI Agent Trust
With a long history of successfully delivering conversation intelligence solutions for highly regulated industries, we have adopted rigorous quality assurance to effectively monitor and measure every AI Agent interaction for quality, compliance, and trust. Drill down reporting, alerting, simulations, and fallbacks give you the ability to deploy and scale with confidence.
04
04
Continuous Learning Loop
By continuously exposing AI Agents to real-world simulations and your actual call interactions, your agents will continue to learn and evolve with your business.
Real results from actual customers





Ready to invest in better member outcomes?
Let us show you how to optimize member service experiences, operations, and compliance with AI Agents powered by leading customer experience AI.
FAQ
Observe.AI helps payers improve member experience by automating high-volume interactions such as benefits questions, eligibility checks, provider search, prescription cost inquiries, and portal support. AI Agents offer 24/7 assistance in multiple languages, helping members access the information they need quickly and accurately.
AI Agents can manage a wide range of payer workflows, including coverage inquiries, in-network provider lookup, prescription eligibility, and digital portal troubleshooting. They also offload routine compliance and validation steps, helping service teams stay focused on higher-value member needs.
Observe.AI enhances every member interaction by providing empathetic, accurate support and by guiding agents with real-time prompts and next-best-actions. This leads to better first-call resolution, improved empathy scores, faster service, and more consistent communication — all of which contribute to better health outcomes and member satisfaction.
Yes. Payers use Observe.AI to automate data entry, enrollment steps, prior authorization form capture, and other administrative tasks that typically extend after-call work. Customers have seen over 32% reduction in after-call work, allowing care teams to spend more time supporting members.
Observe.AI analyzes 100% of member interactions to identify compliance risks, detect service gaps, and uncover reasons for member dissatisfaction or attrition. These insights enable payers to refine workflows, improve quality assurance, reduce operational costs, and ensure regulatory-safe communication at scale.








